| If you cannot view this email, please click here |
|
|
 Baby Friendly Hospital Initiative Hong Kong Association Baby Friendly Hospital Initiative Hong Kong Association |
|
|
|
|
Working towards Baby-friendliness: Why and How?
Lam Chi Oi Christine
Nurse Consultant (Breastfeeding)
Queen Elizabeth Hospital
The Importance of Supporting Breastfeeding Right from the Start
Sustained breastfeeding confers many health benefits to the mother and child. Nowadays, almost 9 out of 10 mothers in Hong Kong start to breastfeed after giving birth. Yet, only less than ⅓ are able to exclusively breastfeed for the first 6 months or so as recommended by the World Health Organization (WHO). Interestingly, the Breastfeeding Survey (Department of Health, 2017) reveals that the biggest drop in exclusive breastfeeding rate occurs within the first month of birth whereas the subsequent decline is much less. For infants born in 2016, the breastfeeding rate on discharge from hospital was 87%, and the exclusive breastfeeding rate at 1, 2 and 4 months were 34%, 33% and 31% respectively.1 This suggests that if mothers are adequately supported to establish exclusive breastfeeding in the early postpartum weeks, breastfeeding in the subsequent months will likely be sustained. In addition to family support, the provision of a conducive environment and effective professional assistance in birthing hospitals and Maternal and Child Health Centres is therefore crucial for mothers to establish successful breastfeeding in the early weeks and subsequent months.
The Baby Friendly Hospital Initiative: Why?
Although breastfeeding is the norm of infant feeding, it is notable that some modern birthing practices and clinical procedures might interfere with breastfeeding, such as the separation of the mother and baby, delaying the start of breastfeeding and unnecessary supplementation of formula milk, etc.
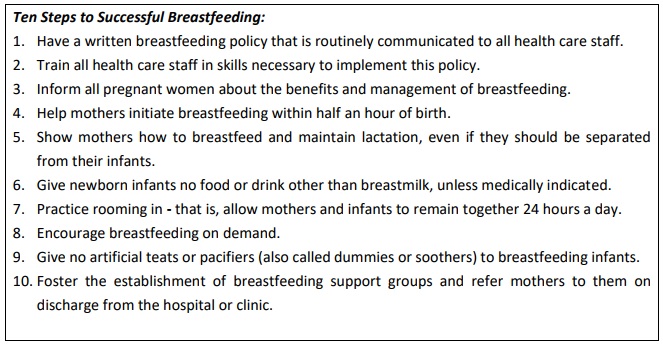
In 1989, the WHO and UNICEF promulgated the “Ten Steps to Successful Breastfeeding” (Ten Steps) as a global standard of quality maternity care. The Ten Steps address maternity facilities’ policies, training, community outreach, and caring procedures for new mothers and babies. The Baby-friendly Hospital Initiative (BFHI) was subsequently launched to encourage maternity facilities worldwide to adopt the Ten Steps. Maternity facilities that document their full adherence to the Ten Steps, as well as compliance with the International Code of Marketing of Breast-milk Substitutes can be designated “Baby-friendly”. To date, more than 152 countries around the world have implemented the initiative. 2
Evidence of Effectiveness of the Ten Steps
Ample evidence has shown that the BFHI improves breastfeeding outcomes. In the 1990s, a group-randomized trial undertaken in Belarus demonstrated an increase in exclusive breastfeeding rate at 3 months to 43% in hospitals that implemented the Ten Steps, compared to only 6% in those not having received the intervention.3 Overseas and local studies have revealed that greater exposure to baby-friendly practices substantially increased new mothers' chances of breastfeeding.4,5 In 2016, a systematic review of 58 studies demonstrated a dose-response relationship between the number of BFHI steps women were exposed to and the likelihood of improved breastfeeding outcomes (early breastfeeding initiation, exclusive breastfeeding at hospital discharge, any breastfeeding and duration of exclusive breastfeeding).6
The QEH’s Experience of Moving towards Baby Friendliness: All things are difficult before they are easy…
Moving towards baby friendliness is rewarding and yet challenging, especially for a maternity unit with high caseloads. It demands leadership, effective communication, collaboration among disciplines and departments, as well as staff openness and flexibility in coping with changes. We would like to share our experience in facilitating early skin-to-skin contact for all mothers and babies, i.e. normal vaginal delivery as well as Caesarian section (Step 4).
To start with, the BFHI team decided to target the low-risk healthy babies in the labour wards. The team first communicated with all staff involved (including the minor staff), explaining to them what skin-to-skin contact meant (i.e. placing the naked baby on the mother’s naked chest shortly after birth) and its benefits to mothers and babies (e.g. giving the baby warmth and emotional security, regulating the baby's heartbeat and breathing, promoting bonding, and helping the initiation of breastfeeding). The team listened to the staff’s concerns and anticipated difficulties in implementation, and together they tackled the challenges one by one. For example, to keep babies warm and safe during the process, the hospital management led by installing heaters and towel warming cabinets and providing pulse oximeter for babies in the labour wards. To allow babies ample time for skin-to- skin contact and breastfeeding initiation, midwives had to re-prioritise the routine care procedures, such as delaying baby weighing and bathing, till completion of the first feeding or later. If the father was the one who accompanied the mother in labour, he would be invited to hold the baby skin-to-skin if the mother’s condition did not permit her to do so.
As the team had gained more experience and confidence in providing skin-to-skin contact for normal healthy babies, it was extended to babies born by Caesarian section. Implementing skin-to-skin contact in mothers having Caesarian section was challenging and inevitably a delicate balancing act between ensuring patient safety and facilitating breastfeeding. Again, the team worked closely with the obstetricians, anaesthetists, paediatricians, nurses and relevant staff in the operating theatre. To ensure mother and baby safety, a midwife was allocated to supervise the process and offer timely support to the mother in the operating theatre and recovery room whenever necessary. With practice, the process was found neither interfering with the operation (by the obstetrician) nor obstructing monitoring of the mother’s condition (by the anaesthetist). Both obstetricians and the anaesthetic team are now happy with babies having skin-to-skin contact with their mothers soon after delivery.
In successfully moving the BFHI forward, it has taken enormous effort, patience, mutual understanding and collaboration of all grades and ranks of staff from different departments and work units.
Key Message:
References:1. Breastfeeding survey 2017. Family Health Service, Department of Health, HKSAR.
2. National Implementation of the Baby-friendly Hospital Initiative, 2017. World Health Organization 2017.
3. Kramer MS, Chalmers B, Hodnett ED, Sevkovskaya Z, Dzikovich I, Shapiro S et al. Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA. 2001;285: 413–20.
4. DiGirolamo AM, Grummer-Strawn LM, Fein SB. Effect of maternity-care practices on breastfeeding. Pediatrics. 2008; 122(Suppl. 2):S43–9. doi:10.1542/peds.2008-1315e.
5. Tarrant, M. (2011). Impact of baby‐friendly hospital practices on breastfeeding in Hong Kong. Birth, 38(3).
6. Pérez-Escamilla R, Martinez JL, Segura-Pérez S. Impact of the Baby-friendly Hospital Initiative on breastfeeding and child health outcomes: a systematic review. Matern Child Nutr. 2016;12(3):402–17. doi:10.1111/mcn.12294.
Views expressed in this article are the author's and do not necessarily reflect the opinion or position of the BFHIHKA.
作者在本文章表達的見解,未必代表愛嬰醫院香港協會的意見或立場
Editor-in-Chief: Dr Shirley Leung
Editorial Team: Ms Georgiana Cheung, Ms Candice Chin, Ms Sing Chu, Ms Christine Lam, Ms Iris Lam, Ms Grace Ma
Please click here to download the whole article and visit our website to subscribe our E-newsletter!
 |
|
|
|
|
|
|
|
Baby Friendly Hotline: 2838 7727 (9am-9pm)
General Enquiry: 2591 0782
Address: 7th Floor, SUP Tower, 75-83 King’s Road, Hong Kong
|
|
|
|
愛嬰醫院香港協會,版權所有。
All rights reserved by Baby Friendly Hospital Initiative Hong Kong Association. |
|
|
|
|