 Baby Friendly Hospital Initiative Hong Kong Association Baby Friendly Hospital Initiative Hong Kong Association |
|
|
|
|
|
Supplementary Feeds in the Early Days: Required or not Required?
Ms Amy Yeung
Midwife Consultant, Lactation Consultant
Department of Obstetrics & Gynecology
Kwong Wah Hospital
Dr Amy FUNG Wai Han
MBBS(HK), Private practitioner
In this article, we are going to describe a mother’s breastfeeding journey during her stay in a hospital maternity unit in the first 72 hours. This will be followed by a commentary on the following at various stages:

- the state of the mother’s milk supply
- whether the baby was getting enough breastmilk
- whether supplementary feeding was necessary
Case History
A healthy first-time mother had expressed her wish to deliver vaginally and breastfeed exclusively. However, she had to undergo an emergency Caesarean Section at 39 weeks’ gestation due to fetal distress 6 hours after the onset of labour. She delivered a healthy baby boy weighing 2.95 Kg. The mother and baby had early skin-to-skin contact in the recovery room although breastfeeding could not be successfully initiated. Rooming-in was the standard practice in the postnatal ward.
The mother was offered coaching in the initial two feeds. She was able to position her baby well on return demonstration (to the nurse). However, she had mild nipple pain during feeding and the nipples looked slightly squashed after feeding. In the first 24 hours, she breastfed her baby 8 times with satisfactory stool and urine output, of which there were 6 meconium stools and one wet diaper by 14 hours after birth. By 35 hours, while there had been 3 more meconium stools, the baby had not yet passed his second urine (i.e. 20 hours since the first) despite breastfeeding every 2-3 hours. The baby’s general condition was good and he was well perfused without signs of dehydration. At this point, the nurse suggested the mother to give 20 ml of formula supplement. The baby passed urine and some greenish stool 4 hours later.
At 48 hours, the baby weighed 2.73 Kg (weight loss of 7.46% since birth). The mother had no feeling of milk coming in. She had fed her baby directly on the breast 9 times in the past 24 hours and the baby had been able to suckle for 25-30 minutes and appeared contented in the majority of the feeds. His general condition was good and there was no sign of dehydration. The mother was encouraged to manually express her breastmilk after feeds and give 15 ml of supplement (expressed breastmilk followed by formula milk) using a cup if the baby was not satisfied after direct breastfeeding.
At 72 hours of life, the baby weighed 2.69 Kg (weight loss of 8.81% since birth). The mother’s milk had still not come in. Within the past 24 hours, the mother had continued to feed on demand (direct breastfeeding for 8 times) and given supplement of 10-15 ml of formula milk 4 times and trace amount (less than 0.5ml) of expressed breast milk twice. The baby had passed 4 greenish stools and 1 yellow stool, and had 4 wet diapers. The mother and baby were discharged at this stage.
Feeding and Output Chart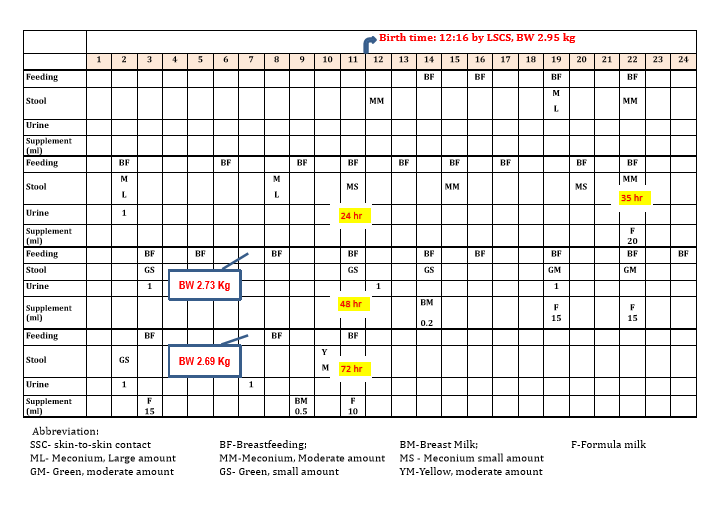
What was the state of the mother’s milk supply?
Lactogenesis II with significant increase in milk volume (milk coming in) usually occurs at 36-72 hours postpartum when a mother often feels fullness or heaviness in the breasts. Delayed lactogenesis II is defined as milk coming in after 72 hours postpartum. Caesarean Section is a risk factor for delayed lactogenesis II due to a lack of stress induced rise in prolactin immediately following birth (Zandaro et al 2012). This mother did not feel breast fullness by 72 hours postpartum. Although the use of analgesics for her Caesarean wound might have reduced her sensation of breast fullness, delayed lactogenesis II was likely.
Was the baby getting enough breastmilk and was supplementation needed?
The baby’s behaviour on the breast such as satiety cues after feeding, feeding frequency, body weight, urinary output and bowel output are all important indicators of how well the baby is feeding. Physiological weight loss of 5-8% in a healthy full term baby during the early neonatal days is common with a trough usually occurring on Day 3. For babies born by Caesarean Section, the weight loss can be up to 10-12% which may occur later. In the first two days, a baby getting enough breastmilk usually has at least 1-2 wet diapers and 1 meconium passed per day. In the third to fourth day, there are at least 3 wet diapers and 2 transitional stools per day.
In the first 24 hours, this baby had passed 6 substantial meconium stools and had one wet diaper. These indicated satisfactory output and thus adequate milk intake.
At 35 hours of age, although there had not been urine output since the first urine at 14 hours, there had been another 5 meconium stools over the subsequent 20 hours. Many international lactation guidelines take urine output, stool output and body weight as the main indicators of a baby’s intake. Focusing on a single parameter, particularly urine output in the early neonatal days, may not be appropriate. It is because urine is normally excreted in small amount in the first 2 days and therefore easily masked by the meconium if they are passed at the same time. Excessive weight loss and inadequate stools are sensitive indicators of inadequate intake among breastfed infants (Oddie 2013 and Moritz 2005). Considering the satisfactory bowel output and good general condition of the baby, he had most probably been getting enough breastmilk. Supplementation had likely not been indicated at this point.
At 48 hours of life, the baby had a few signs suggestive of adequate intake: (1) adequate stool frequency (5 in the past 24 hours); (2) timely appearance of greenish transitional stools; (3) acceptable physiological weight loss of 7.46%; (4) satisfactory general well-being without signs of dehydration; and (5) willingness to take 9 feeds in the past 24 hours. Again, supplementation might not have been indicated at this point. Instead, provision of on-going breastfeeding support for the mother and baby was mandatory because she had increased risk for delayed lactogenesis II and the baby had attachment problem (mother having nipple pain). The baby should be observed closely for signs of dehydration. The mother should be encouraged to breastfeed directly when the baby’s early feeding cues were observed so that the baby is not hungry to the extent of being irritable, thus facilitating better positioning and attachment. In addition to increasing skin-to-skin contact, helping the mother to relax with adequate pain relief would be essential to promote oxytocin release.
At 72 hours of life, the mother’s milk still had not come in. Mothers with delayed lactogenesis II are prone to breastfeeding problems, such as baby’s significant weight loss, hypernatraemia, hyperbilirubinaemia, lack of maternal confidence and premature stopping of breastfeeding. Despite supplementation of 55 ml of formula milk and trace amount of expressed breast milk in the past 24 hours, the baby’s weight loss had increased to 8.81% which was slightly above the normal range. At this point, the mother and her baby were discharged. In view of the mother’s delayed lactogenesis II, attachment problem and the baby’s borderline weight loss on day 3, advice on short term supplementation for this baby before discharge was justifiable.
Further Discussion on “The Science and Art of Supplementation"
Healthy term newborns have adequate energy reserve in the form of hepatic glycogen, protein and fat. They have the ability to maintain their blood glucose level via glycogenolysis and gluconeogenesis, as well as to utilize ketone bodies (from fat metabolism) as an alternative energy source. Hence, they are at low risk of hypoglycemia in the first 48 hours of life despite the small amount of colostrum. Unless there are significant problems in output, weight loss, suckling or general well-being, healthy term newborns likely do not need supplementation in the first 2 days.
Although supplementation might not have been absolutely indicated in the first 2 days in this baby, it does have its role to play in the busy hospital setting where manpower allocation in close monitoring and supporting the mother-baby dyad may not be forthcoming. Besides, to ensure that healthy babies can be discharged without undue delay, a wider safety margin for action like supplementing a baby with marginal weight loss or urine output may be needed.
To prevent complications of anticipated probable inadequate intake, it was of utmost importance that the mother clearly understood the following before going home: (1) how to monitor urinary and bowel output; (2) when to supplement (i.e. when output is unsatisfactory or when the baby is not satisfied right after direct breastfeeding); (3) how much to supplement; (4) what to supplement (the first choice is expressed breastmilk); (5) how to give supplement (the first choice is by cup); and (6) follow up at an MCHC or lactation clinic of the hospital within 2 days of discharge. With prompt post-discharge professional support, it could be expected that the mother’s milk production would upregulate and baby’s suckling would become more effective so that supplementation could be weaned off gradually.
Key Message:
References:
Oddie SJ et al. Severe neonatal hypernatraemia: a population based study. Arch Dis child Neonatal Ed. 2013; 0:F1-F4
Moritz L et al. Breastfeeding-associated hypernatraemia: are we missing the diagnosis? Pediatrics 2005; 116:343-347
Views expressed in this article are the author's and do not necessarily reflect the opinion or position of the BFHIHKA.
作者在本文章表達的見解,未必代表愛嬰醫院香港協會的意見或立場
Editor-in-Chief: Dr Shirley SL Leung
Editorial Team: Dr Amy Fung, Ms Iris Ip, Ms Helen Leung, Ms Agnes Wong, Dr Sandra Yau, Ms Amy Yeung

|
|
|
|
|
|
|
|
Baby Friendly Hotline: 2838 7727 (9am-9pm)
General Enquiry: 2591 0782
Address: 7th Floor, SUP Tower, 75-83 King’s Road, Hong Kong
|
|
|
|
愛嬰醫院香港協會,版權所有。
All rights reserved by Baby Friendly Hospital Initiative Hong Kong Association.
|
|
|
|
|